Authors: Hadar Bootz-Maoz, Ayelet Pearl, Ehud Melzer, Stephen Malnick, Efrat Sharon, Yifat Bennet, Rotem Tsentsarevsky, Shlomi Abuchatzera, Sivan Amidror, Elana Aretz, Shalhevet Azriel, Chen Gam Ze Letova, Maria Naama, Irit Shoval, Orly Yaron, Sarit Karako-Lampert, Shai Bel, Nissan Yissachar
Cell Reports, Volume 41, Issue 7, 2022
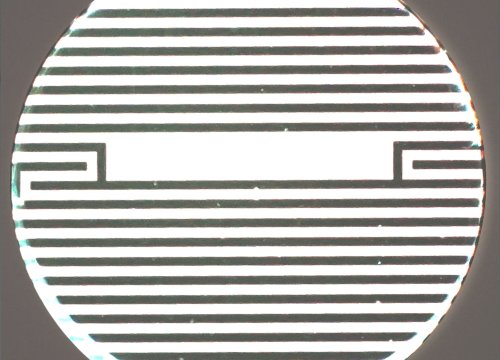
Scientists perform TEER measurements to evaluate epithelial tissue and barrier integrity in IBS using Axion’s noninvasive, label-free Maestro platform with Impedance Module.
Research has demonstrated that eating a low-FODMAP (fermentable oligo-, di-, mono-saccharides and polyols) diet alters the composition of the gut microbiome and leads to a clinical response in some people with irritable bowel syndrome (IBS), but the impact of specific microbial taxa on host tissues is not well understood. In this study, scientists developed a gut organ culture system and used a multiplatform approach to investigate colonic responses to microbiota communities in people with IBS before and after consuming a low-FODMAP diet.
After showing that the low-FODMAP diet reduced B. adolescentis abundance, and based on previous evidence, the authors hypothesized that the organism may disrupt epithelial cell integrity and gut barrier functions in IBS. To evaluate this premise, the researchers used Axion’s noninvasive, label-free Maestro Edge system with the Impedance Module to measure TEER in colonic epithelial cells cultured with different bacteria in vitro and showed that B. adolescentis impaired epithelial barrier integrity. Taken together with other results, the authors suggest that the findings “support the hypothesis that the gut microbiota mediates the beneficial effects of a low-FODMAP diet and reinforce the potential feasibility of microbiome-based therapies in IBS.”